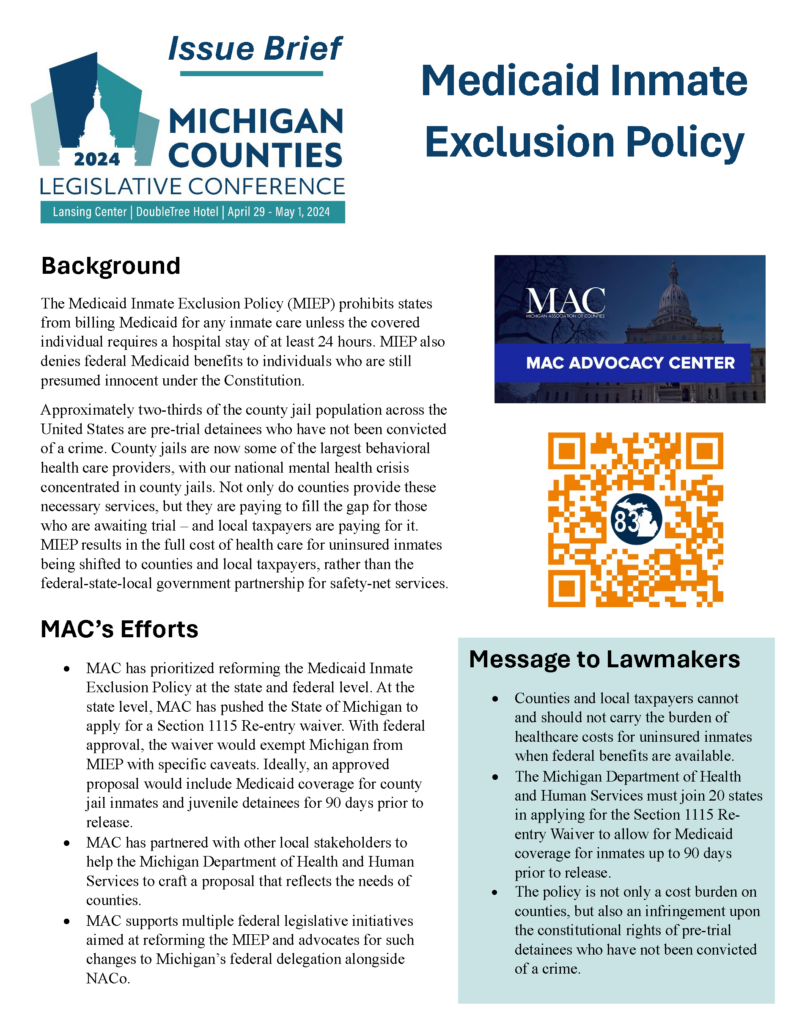
Medicaid Inmate Exclusion Policy - Medicaid inmate exclusion policy prevents them from having benefits and care plans in place to continue treatment immediately upon release. When medicaid was authorized in 1965, the “inmate exclusion policy” was established to prevent state and local. Medicaid can pay for services provided during an inpatient stay of at least 24 hours in a medical institution, such as an acute. In a new explainer, kff examines a new waiver opportunity that allows states to request a partial waiver of the inmate exclusion. The medicaid inmate exclusion policy, which blocks states from using medicaid funds for health care in jails and prisons, makes. The “inmate exclusion policy” has prohibited federally funded health insurance programs, including medicaid, from financing care for.
Medicaid inmate exclusion policy prevents them from having benefits and care plans in place to continue treatment immediately upon release. In a new explainer, kff examines a new waiver opportunity that allows states to request a partial waiver of the inmate exclusion. Medicaid can pay for services provided during an inpatient stay of at least 24 hours in a medical institution, such as an acute. The “inmate exclusion policy” has prohibited federally funded health insurance programs, including medicaid, from financing care for. The medicaid inmate exclusion policy, which blocks states from using medicaid funds for health care in jails and prisons, makes. When medicaid was authorized in 1965, the “inmate exclusion policy” was established to prevent state and local.
The “inmate exclusion policy” has prohibited federally funded health insurance programs, including medicaid, from financing care for. The medicaid inmate exclusion policy, which blocks states from using medicaid funds for health care in jails and prisons, makes. When medicaid was authorized in 1965, the “inmate exclusion policy” was established to prevent state and local. Medicaid inmate exclusion policy prevents them from having benefits and care plans in place to continue treatment immediately upon release. In a new explainer, kff examines a new waiver opportunity that allows states to request a partial waiver of the inmate exclusion. Medicaid can pay for services provided during an inpatient stay of at least 24 hours in a medical institution, such as an acute.
Counties continue efforts to address the Medicaid Inmate Exclusion
The “inmate exclusion policy” has prohibited federally funded health insurance programs, including medicaid, from financing care for. In a new explainer, kff examines a new waiver opportunity that allows states to request a partial waiver of the inmate exclusion. When medicaid was authorized in 1965, the “inmate exclusion policy” was established to prevent state and local. Medicaid inmate exclusion policy.
NACoNSA Joint Task Force Report Addressing the Federal Medicaid
The “inmate exclusion policy” has prohibited federally funded health insurance programs, including medicaid, from financing care for. In a new explainer, kff examines a new waiver opportunity that allows states to request a partial waiver of the inmate exclusion. Medicaid inmate exclusion policy prevents them from having benefits and care plans in place to continue treatment immediately upon release. When.
NACoNSA Joint Task Force Report Addressing the Federal Medicaid
When medicaid was authorized in 1965, the “inmate exclusion policy” was established to prevent state and local. The “inmate exclusion policy” has prohibited federally funded health insurance programs, including medicaid, from financing care for. The medicaid inmate exclusion policy, which blocks states from using medicaid funds for health care in jails and prisons, makes. Medicaid can pay for services provided.
NACoNSA Joint Task Force Report Addressing the Federal Medicaid
When medicaid was authorized in 1965, the “inmate exclusion policy” was established to prevent state and local. Medicaid inmate exclusion policy prevents them from having benefits and care plans in place to continue treatment immediately upon release. The medicaid inmate exclusion policy, which blocks states from using medicaid funds for health care in jails and prisons, makes. Medicaid can pay.
Check out MAC Issue Briefs on key policy battles in Lansing The
In a new explainer, kff examines a new waiver opportunity that allows states to request a partial waiver of the inmate exclusion. Medicaid can pay for services provided during an inpatient stay of at least 24 hours in a medical institution, such as an acute. The medicaid inmate exclusion policy, which blocks states from using medicaid funds for health care.
Exclusion List Medicaid An Ultimate Guide — Etactics
The “inmate exclusion policy” has prohibited federally funded health insurance programs, including medicaid, from financing care for. Medicaid can pay for services provided during an inpatient stay of at least 24 hours in a medical institution, such as an acute. When medicaid was authorized in 1965, the “inmate exclusion policy” was established to prevent state and local. The medicaid inmate.
End the Medicaid Inmate Exclusion Policy — YourPath
Medicaid inmate exclusion policy prevents them from having benefits and care plans in place to continue treatment immediately upon release. When medicaid was authorized in 1965, the “inmate exclusion policy” was established to prevent state and local. In a new explainer, kff examines a new waiver opportunity that allows states to request a partial waiver of the inmate exclusion. The.
NACoNSA Joint Task Force Report Addressing the Federal Medicaid
Medicaid inmate exclusion policy prevents them from having benefits and care plans in place to continue treatment immediately upon release. The “inmate exclusion policy” has prohibited federally funded health insurance programs, including medicaid, from financing care for. Medicaid can pay for services provided during an inpatient stay of at least 24 hours in a medical institution, such as an acute..
Medicaid Inmate Exclusion Policy In Powerpoint And Google Slides Cpb
The “inmate exclusion policy” has prohibited federally funded health insurance programs, including medicaid, from financing care for. In a new explainer, kff examines a new waiver opportunity that allows states to request a partial waiver of the inmate exclusion. The medicaid inmate exclusion policy, which blocks states from using medicaid funds for health care in jails and prisons, makes. Medicaid.
NACoNSA Joint Task Force Report Addressing the Federal Medicaid
The medicaid inmate exclusion policy, which blocks states from using medicaid funds for health care in jails and prisons, makes. When medicaid was authorized in 1965, the “inmate exclusion policy” was established to prevent state and local. Medicaid inmate exclusion policy prevents them from having benefits and care plans in place to continue treatment immediately upon release. In a new.
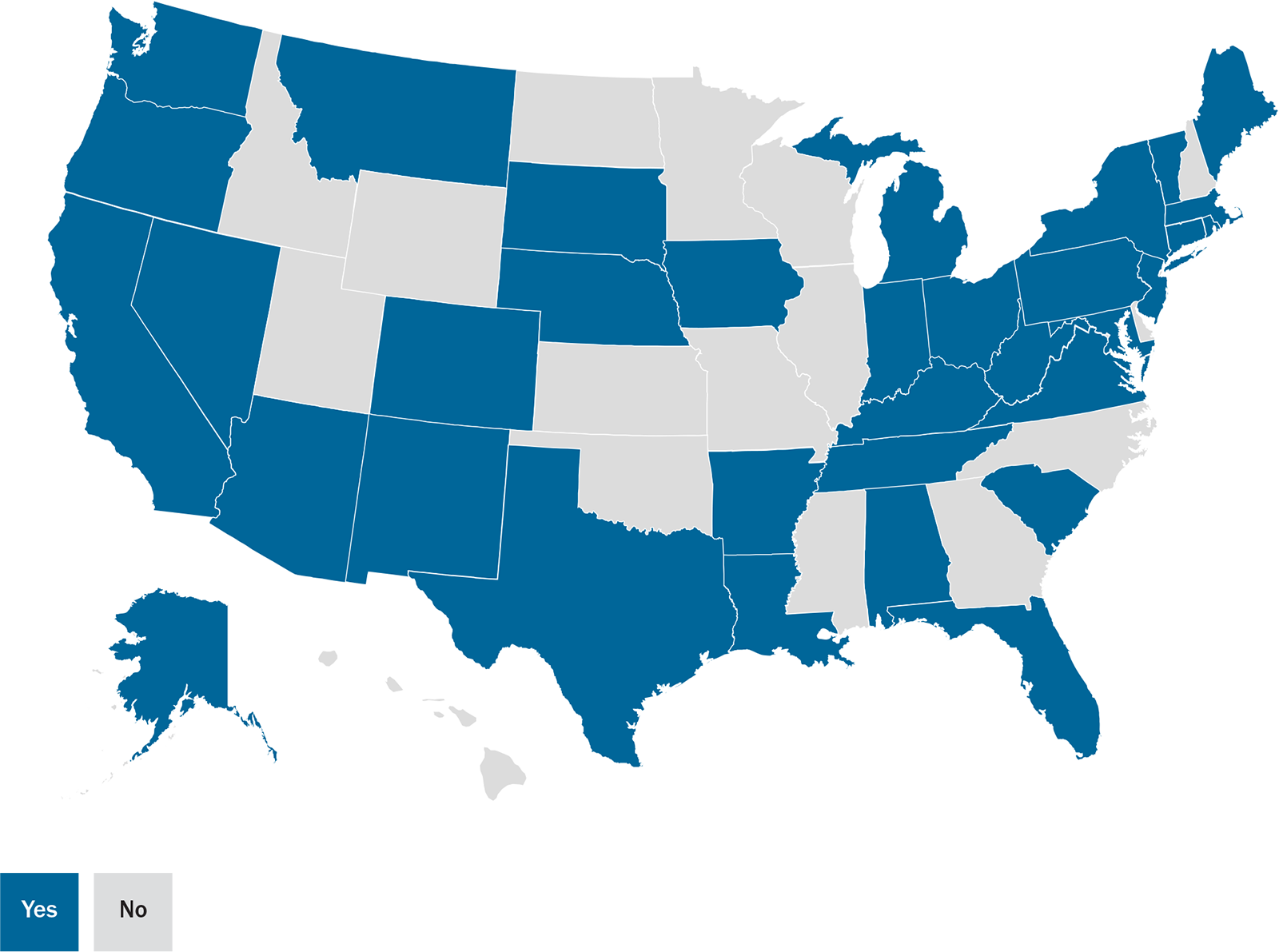
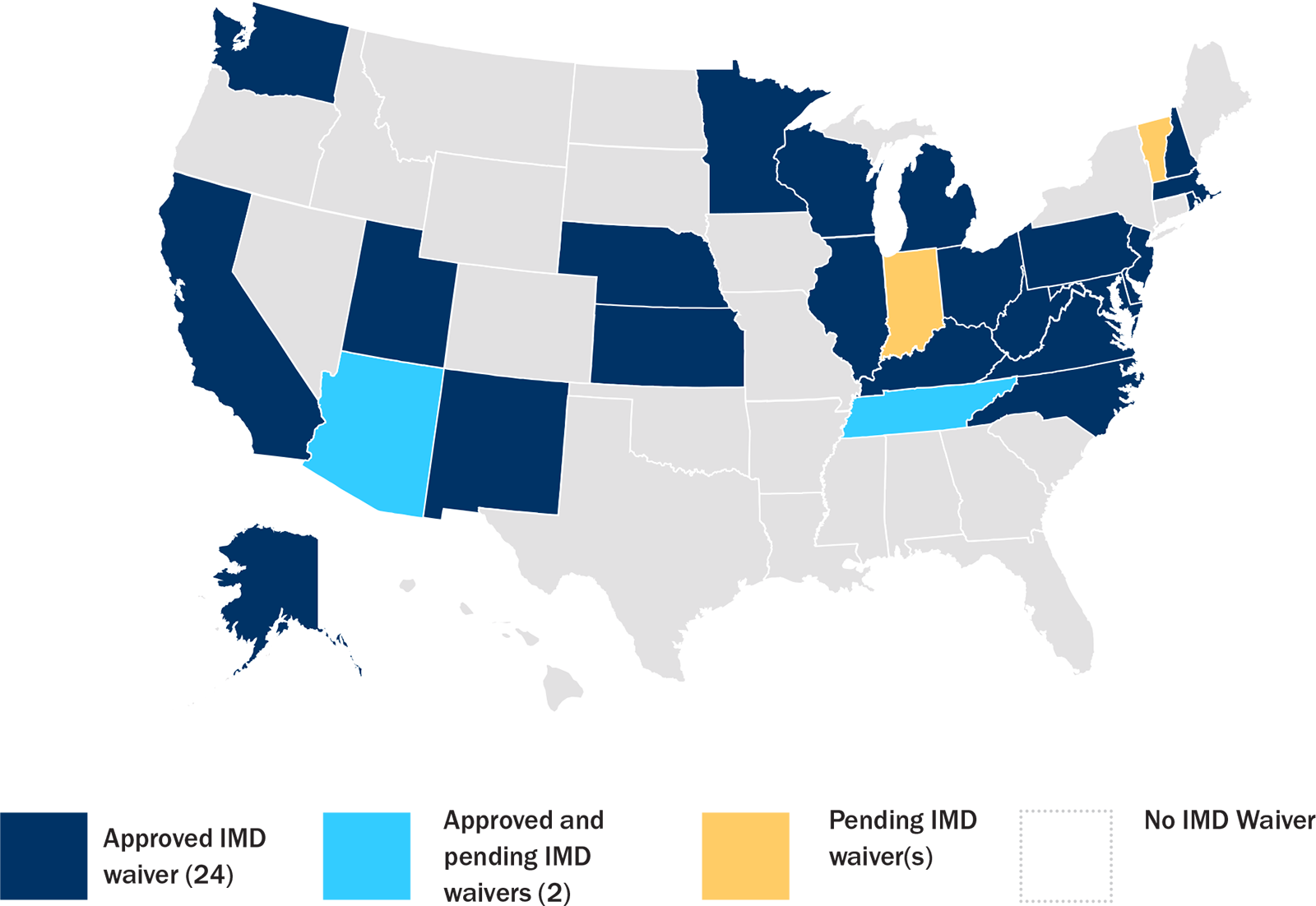
In A New Explainer, Kff Examines A New Waiver Opportunity That Allows States To Request A Partial Waiver Of The Inmate Exclusion.
The “inmate exclusion policy” has prohibited federally funded health insurance programs, including medicaid, from financing care for. When medicaid was authorized in 1965, the “inmate exclusion policy” was established to prevent state and local. Medicaid can pay for services provided during an inpatient stay of at least 24 hours in a medical institution, such as an acute. Medicaid inmate exclusion policy prevents them from having benefits and care plans in place to continue treatment immediately upon release.